- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Mean Platelet Volume independently Linked to Mortality among Peritoneal Dialysis Patients
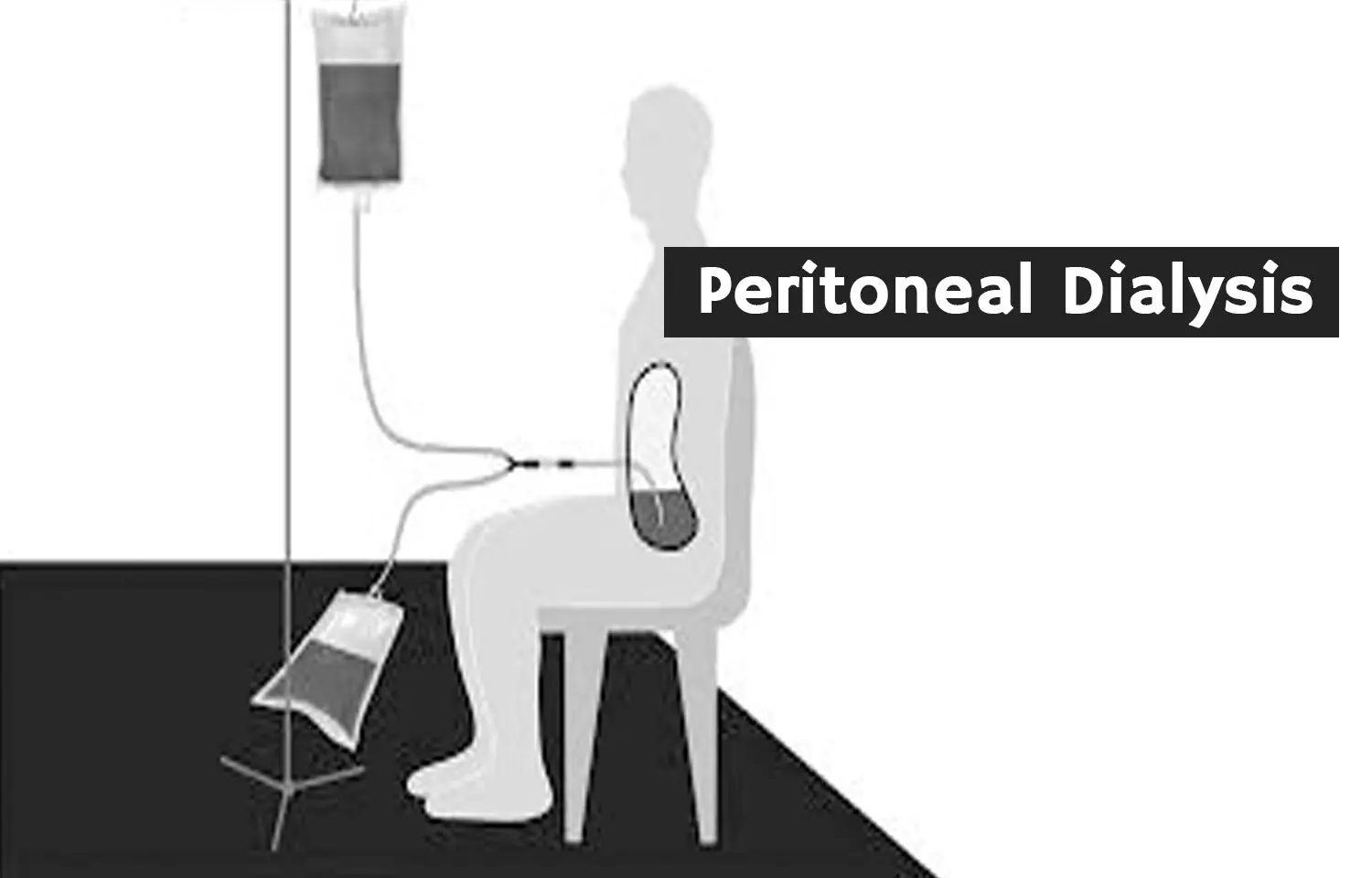
In a groundbreaking exploration at the intersection of platelet volume and patient outcomes, a recent study has illuminated the potential role of mean platelet volume (MPV) as a significant indicator of mortality risks in individuals undergoing peritoneal dialysis (PD). While MPV has previously been associated with severity and mortality in sepsis patients, this study expands its relevance to the realm of renal care. The study found that MPV is independently associated with both all-cause mortality and cardiovascular mortality in patients undergoing peritoneal dialysis.
The study results were published in the journal BMC Cardiovascular Diseases.
In the realm of medical research, the mean platelet volume (MPV) has emerged as a valuable indicator, demonstrating associations with severity and all-cause mortality in patients with sepsis. However, a recent study has delved into uncharted territory, exploring the relationship between MPV and all-cause mortality, as well as cardiovascular mortality, in patients undergoing peritoneal dialysis (PD). The primary objectives of this retrospective study were to uncover the potential links between MPV and both all-cause mortality and cardiovascular mortality among patients treated with PD.
Researchers retrospectively gathered data from 1,322 patients undergoing PD between November 1, 2005, and August 31, 2019. The study's primary outcomes were identified as all-cause mortality and cardiovascular mortality. To classify MPV, the researchers employed the X-tile software. The correlation between MPV and mortality was assessed using Cox models, and survival curves were generated using the Kaplan-Meier method.
Key Findings:
- The median follow-up period for the study participants was 50 months (ranging from 30 to 80 months), during which a total of 360 deaths were recorded.
- For all-cause mortality, patients with MPV ≥ 10.2 fL exhibited a significantly higher risk across three different models.
- Furthermore, PD patients with MPV ≥ 10.2 fL demonstrated a notably elevated risk of cardiovascular mortality in all three models.
This groundbreaking study concludes that MPV is independently associated with both all-cause mortality and cardiovascular mortality in patients undergoing peritoneal dialysis. These findings offer valuable insights into the potential role of MPV as a prognostic marker for mortality risks in the context of PD.
The implications of this research extend beyond the specific patient population studied, prompting further exploration of MPV as a potential biomarker in other medical contexts. As the scientific community continues to uncover the intricate relationships between platelet volume and health outcomes, these findings open new avenues for understanding and managing mortality risks in diverse patient groups.
Further reading: Mean platelet volume and the association with all-cause mortality and cardiovascular mortality among incident peritoneal dialysis patients. https://doi.org/10.1186/s12872-023-03551-x
BDS, MDS
Dr.Niharika Harsha B (BDS,MDS) completed her BDS from Govt Dental College, Hyderabad and MDS from Dr.NTR University of health sciences(Now Kaloji Rao University). She has 4 years of private dental practice and worked for 2 years as Consultant Oral Radiologist at a Dental Imaging Centre in Hyderabad. She worked as Research Assistant and scientific writer in the development of Oral Anti cancer screening device with her seniors. She has a deep intriguing wish in writing highly engaging, captivating and informative medical content for a wider audience. She can be contacted at editorial@medicaldialogues.in.




